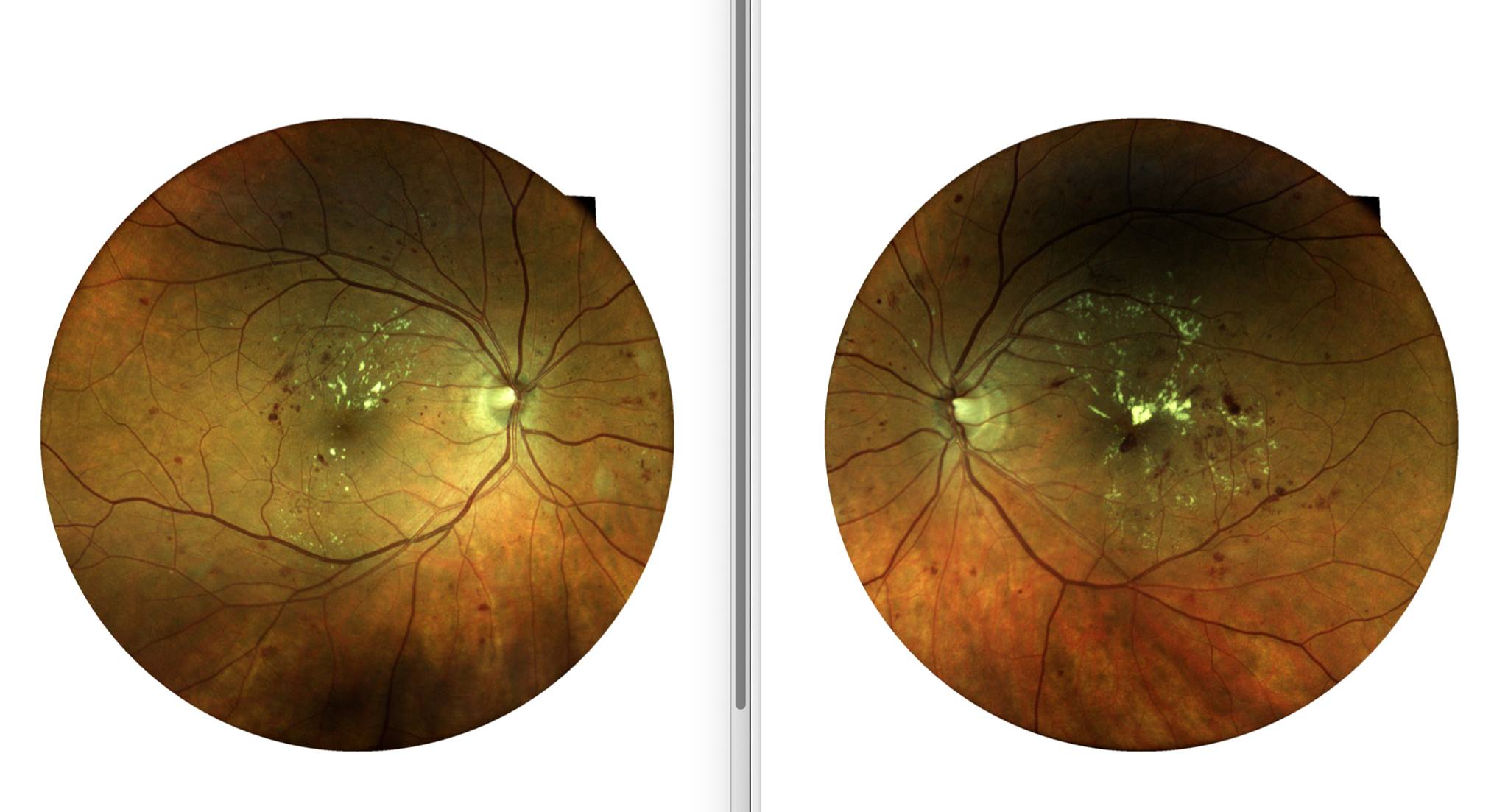
The retinae of a white female in her early 50s who received LASIK vision correction about 15 years ago. In the intervening 15 years, she received only a few eye exams and none performed by a medically focused optometry office. To the contrary, she received only exams performed by franchise optometrists who quickly dispensed an Rx to sell her glasses. This patient appeared very healthy, not obese, but admitted to rarely visiting her PCP for physical exams. Based on the severity of the diabetic retinopathy, it is estimated she has had diabetes for years and years, possibly up to a decade. Her best corrected visual acuity was 20/30 in the right eye and 20/40 in the left eye. Further degradation of her vision puts at risk her privilege to drive a car (as defined by the state, not by the optometrist).
This photo was taken by Dr. Son Nguyen on a Centervue Compass which uses confocal microscopy technology to produce a true color accurate photograph of the retinae.
Diabetic Retinopathy
Diabetic retinopathy is the leading cause of preventable blindness in the United States. According to a study by the Center for Disease control, an estimated more than 100 million US adults (roughly 1/3rd the population) is living with diabetes or pre-diabetes.(1)
It is important that patients with diabetes receive comprehensive medical eye exams yearly. A medical eye exam is different from a routine eye exam in several ways. The main difference is that diabetic medical eye exams include dilations and retinal photos.
The American Diabetes Association recommends patients with diabetes receive a diabetic medical eye exam yearly whereby an optometrist will inspect the retina for damage caused by diabetes. The ADA guidelines recommends a patient with diabetes receive a dilated fundus exam and retinal photograph once every two years until damage from diabetic retinopathy is observed. Once diabetic retinopathy is observed, the ADA guideline recommends yearly dilated fundus exams with retinal photos.
Some optometrists and doctors may deviate from these guidelines. At Morgan Hill Eyecare Optometry, Dr. Son likes the guidelines up to around year ten of diabetes. Empirical evidence and studies show that diabetic retinopathy becomes more prevalent as the number of years of diabetes increases. Around the tenth year of diabetes, Dr. Son likes to dilate yearly regardless of whether diabetic retinopathy is present.
Diabetic retinopathy most commonly manifests itself as tiny dot bleeds in the retina (the delicate sliver of brain tissue that senses light and then sends the light signal as chemical-electrical impulses to the brain). Blood and brain tissue should not mix and to prevent that mixing in the brain is the purpose of the Blood/Brain Barrier. Similarly, present in the eyes is a Blood/Retina Barrier. Bleeds in the retina are breaks in that barrier and as blood interacts with the rods and cones (the light-sensing neurons of the eyes), the rods and cones slowly die leaving tiny blind spots that lead to blur and eventual blindness if left untreated.
Sources:
1) https://www.cdc.gov/media/releases/2017/p0718-diabetes-report.html